Chronic low-grade inflammation (or chronic silent inflammation)
Highlight – Why this is a central topic
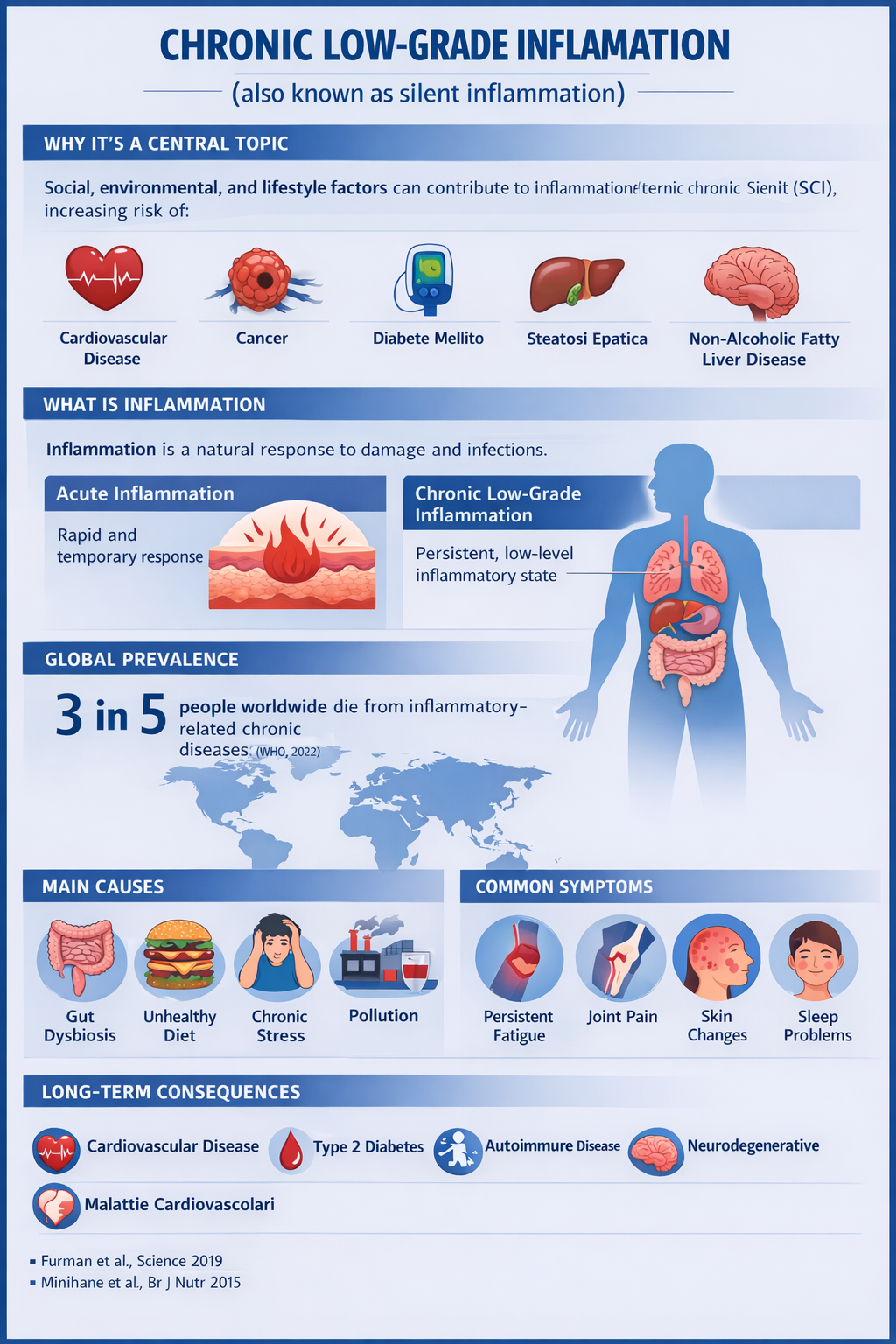
Although intermittent increases in inflammation are essential for survival during physical injury and infection, recent research has revealed that certain social, environmental, and lifestyle-related factors can promote systemic chronic inflammation (SCI), which in turn may lead to a variety of diseases that collectively represent the leading causes of disability and mortality worldwide, such as cardiovascular disease, cancer, diabetes mellitus, chronic kidney disease, non-alcoholic fatty liver disease, and autoimmune and neurodegenerative diseases.
References
Furman et al., Science, 2019
Calder et al., Nutrients, 2017
What is inflammation
Inflammation is a central component of innate (nonspecific) immunity. In general terms, inflammation is a local response to cellular damage characterized by increased blood flow, capillary dilation, leukocyte infiltration, and localized production of a series of chemical mediators that contribute to the elimination of toxic agents and the repair of damaged tissues.
It is now clear that the termination (also known as resolution) of inflammation is an active process involving cytokines and other anti-inflammatory mediators, particularly lipid mediators, rather than a simple shutdown of pro-inflammatory pathways.
Inflammation acts both as a “friend and a foe”: it is an essential component of immune surveillance and host defense; however, a persistent inflammatory state over time is a pathological feature of a wide range of chronic conditions.
References
Medzhitov, Nature, 2008
Serhan et al., Nature, 2007
Acute inflammation
Acute inflammation is the body’s rapid, short-term response to injury or infection, characterized by redness, swelling, heat, and pain. It is a beneficial process that helps protect against pathogens and initiates tissue repair. Although it may last from a few hours to a few days, it differs from chronic inflammation, which persists for longer periods and can be harmful.
(Personal note: The classic signs of acute inflammation—heat, redness, swelling, pain—indicate that the body is fighting and healing.)
References
Abbas et al., Cellular and Molecular Immunology
Serhan et al., Nature, 2007
Chronic low-grade inflammation
Low-grade, or “silent,” inflammation is a chronic, non-infectious, low-intensity immune response that persists for months or years. It is often triggered by obesity, metabolic stress, and poor nutrition, which includes not only unhealthy food choices but also incomplete digestive processes and microbiota imbalances.
This condition is characterized by slightly elevated blood markers that are often technically within normal ranges (such as CRP), making clinical diagnosis extremely challenging. It acts as a “silent killer,” serving as a precursor to serious conditions such as diabetes, heart disease, and chronic pain.
Key aspects of low-grade inflammation include:
Multifactorial causes:
In addition to physical inactivity and environmental factors, metabolic disturbances and alterations of the intestinal barrier play a crucial role. When food is not properly digested, it can trigger a persistent immune reaction that fuels the inflammatory state.
Systemic impact:
This chronic state causes mild but continuous tissue damage, directly linked to diseases such as Alzheimer’s disease, type 2 diabetes, cardiovascular disorders, and certain cancers.
How to diagnose it:
A. First phase:
Because standard tests do not detect acute abnormalities, diagnosis must rely on analysis of persistent symptoms such as unexplained fatigue, chronic pain, and cognitive changes (brain fog).
B. Second phase:
High-sensitivity C-reactive protein (hs-CRP) blood test. Unlike standard CRP, hs-CRP can measure values below 0.3 mg/dL, allowing detection of minimal fluctuations that would otherwise remain invisible.
C. Third phase
Interlukin-6 (IL-6). This is a specialized test. In most laboratories, IL-6 is considered “normal” up to about 5–10 pg/mL. In acute infection, IL-6 can rise to 100 or 1000 pg/mL.
In low-grade inflammation, IL-6 may increase from 1 to 3 pg/mL.
Although tripled (and therefore abnormal), the laboratory result will still read “Below limit: NORMAL.” This is why it is an “elusive” marker for general practitioners, but an “advanced biomarker” for specialists who can interpret subtle variations. Specialists often evaluate IL-6 together with the Neutrophil-to-Lymphocyte Ratio (NLR), a simple calculation from the complete blood count that confirms whether the immune system is in a state of chronic alert.
References
Minihane et al., British Journal of Nutrition, 2015
Hotamisligil, Nature, 2006
Pearson et al., Circulation, 2003
Lucius, Integrative and Complementary Therapies, 2023
Low-grade chronic inflammation and systemic inflammation
When the inflammatory state simultaneously involves multiple body districts, it is referred to as systemic inflammation. This condition may arise either from the generalization of an acute inflammatory process or from the progressive extension of an initially localized low-grade chronic inflammatory state.
The intestine represents one of the main sites of origin due to its extensive surface area, intense immune activity, and interaction with the microbiota. However, the process affects numerous organs and tissues.
References
Furman et al., Science, 2019
Franceschi et al., Cell, 2018
Global prevalence
Chronic inflammatory diseases are the leading cause of death worldwide. It is estimated that about 3 out of 5 people globally die from diseases linked to chronic inflammatory processes.
“Chronic inflammatory diseases are the most significant cause of death in the world. The World Health Organization (WHO) ranks chronic diseases as the greatest threat to human health. The prevalence of diseases associated with chronic inflammation is anticipated to increase persistently for the next 30 years in the United States. in 2000, nearly 125 million Americans were living with chronic conditions and 61 million (21%) had more than one. In recent estimates by Rand Corporation, in 2014 nearly 60% of Americans had at least one chronic condition, 42% had more than one and 12% of adults had 5 or more chronic conditions. Worldwide, 3 of 5 people die due to chronic inflammatory diseases like stroke, chronic respiratory diseases, heart disorders, cancer, obesity, and diabetes. 2022”.
References
Furman et al., Science, 2019
Main causes and triggering factors
Gut dysbiosis: Alteration of the intestinal bacterial flora, which may be caused by an unbalanced diet, excessive use of antibiotics, or other toxic substances.
Unhealthy diet: Excessive consumption of processed foods rich in refined sugars and saturated fats, which can promote inflammation.
Stress: Chronic stress can negatively affect the immune system and increase susceptibility to inflammation.
Environmental pollution and toxins: Exposure to chemicals present in the environment or in food may contribute to oxidative stress and inflammation.
Smoking and alcohol: These factors can worsen oxidative stress and damage cells, thereby promoting inflammation.
References
Cani et al., Diabetes, 2007
Tilg & Moschen, Gut, 2014
Egger & Dixon, AJPM, 2014
Slavich & Irwin, Psychological Bulletin, 2014
Common symptoms
Digestive disorders: Bloating, abdominal cramps, diarrhea or constipation, which may vary in intensity and frequency.
Persistent fatigue: Chronic tiredness, lack of energy, and difficulty concentrating.
Joint pain: Widespread muscle and joint pain.
Skin alterations: Rashes, eczema, or other skin manifestations.
Sleep problems: Difficulty falling asleep or maintaining deep sleep.
Skin manifestations
References
Dantzer et al., Brain Behav Immun, 2008
Miller et al., Biol Psychiatry, 2009
Long-term consequences
If left untreated, low-grade intestinal inflammation may contribute to the development of chronic diseases such as:
Cardiovascular diseases: Increased risk of heart attack, stroke, and other cardiovascular conditions.
Type 2 diabetes: Higher likelihood of developing insulin resistance and diabetes.
Autoimmune diseases: Increased susceptibility to conditions such as rheumatoid arthritis, lupus, etc.
Neurodegenerative disorders: Increased risk of developing diseases such as Alzheimer’s or Parkinson’s.
Certain types of cancer: Increased risk of developing some cancers.
General measures that may help reduce inflammation
Follow a balanced diet: Rich in fiber, fruits, vegetables, and whole foods, with a low glycemic index.
Reduce intake of processed foods, refined sugars, and saturated fats.
Manage stress: Through relaxation techniques, meditation, yoga, or other stress-reducing activities.
Maintain a healthy weight: Obesity and overweight can increase inflammation.
Limit alcohol consumption and quit smoking.
Supplement with probiotics: They may help restore the balance of the intestinal bacterial flora.
References
Estruch et al., NEJM, 2018
Calder et al., Br J Nutr, 2011
Note
Low-grade chronic inflammation (or “silent” inflammation) is a key factor in the development and progression of cardiovascular diseases, including atherosclerosis, hypertension, and myocardial infarction. This often asymptomatic process causes endothelial dysfunction, stimulates the formation and rupture of atherosclerotic plaques, and may lead to acute coronary syndromes.
References
Ridker et al., NEJM, 2017
Libby, Nature, 2002
Topics covered in the in-depth study
1 – Paradigmatic cases (Obesity, Metabolic syndrome, Rheumatoid arthritis (autoimmune disease), Biomarkers.
2 – Appendix A: Generalized inflammation
3 – Appendix B: Undigested food
4 – A special case: the role of gluten
2 – Appendix A
Generalized inflammation, also known as systemic inflammation, is a condition in which the inflammatory process simultaneously involves multiple body districts rather than remaining confined to a specific site. This means that inflammatory mechanisms—normally activated as a protective response to infections, injuries, or tissue damage—remain diffusely and persistently active.
Systemic inflammation can develop in two main ways, characterized by different mechanisms, onset times, and clinical significance. On the one hand, it may result from the generalization of an initially localized acute inflammation; on the other, it may arise from the progressive extension of a low-grade chronic inflammatory state, which over time becomes systemic.
In the first case, inflammation begins at a specific site—such as pneumonia, appendicitis, or an infected wound—and rapidly spreads throughout the body. This occurs due to the massive release of inflammatory mediators, including cytokines (such as TNF-α, IL-1, IL-6), prostaglandins, and other pro-inflammatory molecules that enter the circulation, producing a generalized response. Typical examples include sepsis, septic shock, extensive burns, and major trauma. This form—known as acute systemic inflammation or SIRS (Systemic Inflammatory Response Syndrome)—is characterized by rapid onset, high intensity, and marked symptoms such as high fever, tachycardia, hypotension, and major metabolic alterations.
In the second case, inflammation is slow, persistent, and low-intensity. It initially affects one or more specific tissues—such as adipose tissue, the gut, or the joints—and later tends to spread systemically. The underlying mechanism is the continuous production of small amounts of inflammatory mediators that do not trigger an evident acute response but progressively accumulate over time. This condition is termed chronic low-grade systemic inflammation and is frequently associated with obesity, type 2 diabetes, metabolic syndrome, cardiovascular disease, and autoimmune disorders.
Among the main sites of origin of low-grade chronic inflammation, the gut plays a central role due to its large surface area, intense immune activity, and close interaction with the microbiota. Alterations in the intestinal barrier and microbial composition can promote the translocation of pro-inflammatory molecules into the bloodstream, contributing to the systemic spread of the process.
The causes of systemic inflammation—especially in its chronic form—are multiple and include chronic or recurrent infections, obesity, chronic inflammatory diseases such as rheumatoid arthritis and ulcerative colitis, chronic stress, an unbalanced diet rich in saturated fats, sugars, and ultra-processed foods, deficiencies of vitamins, minerals, and antioxidants, as well as smoking and excessive alcohol consumption.
Symptoms of generalized inflammation may vary depending on the cause and severity, but frequently include chronic fatigue, widespread muscle and joint pain, difficulties with concentration and memory, mood swings with irritability, anxiety or depression, digestive disturbances such as constipation or diarrhea, and in some cases a mild, persistent fever.
Over the long term, systemic inflammation represents an important risk factor for numerous chronic diseases, including cardiovascular disease (hypertension, atherosclerosis, myocardial infarction), type 2 diabetes, certain cancers (especially colon and breast), kidney disease, and worsening of autoimmune conditions.
In summary, systemic inflammation can reflect either an acute response that becomes generalized or the outcome of a low-grade chronic process that progressively extends. Although these are different conditions, both involve the simultaneous involvement of multiple organs and systems and have a relevant impact on overall health.
3 – Appendix B
Undigested food
Undigested food can trigger chronic low-grade inflammation, a biological process known as metabolic endotoxemia.
Here are the main mechanisms linking impaired digestion to inflammation:
1. “Leaky gut” (intestinal permeability)
When food macromolecules are not properly broken down (due to enzyme deficiency or insufficient chewing), they can damage the intestinal tight junctions.
Mechanism: Fragments of undigested proteins and bacterial toxins (LPS) pass directly into the bloodstream.
Response: The immune system recognizes these particles as “intruders,” activating a persistent but mild systemic inflammatory response.
2. Dysbiosis and fermentation
Undigested food reaching the colon becomes a substrate for fermentation by pathogenic bacteria.
Protein putrefaction: If proteins are not digested in the stomach/small intestine, their breakdown in the colon produces toxic metabolites such as ammonia and hydrogen sulfide, which irritate the intestinal mucosa and increase pro-inflammatory cytokine levels.
Excess LPS: Overgrowth of Gram-negative bacteria increases lipopolysaccharides (LPS), among the most powerful activators of low-grade inflammation detectable via hs-CRP.
3. Non–IgE-mediated food intolerances
Unlike acute allergies, constant exposure to foods the body cannot properly process (e.g., lactose or fructose malabsorption) keeps the immune system in a state of chronic alert.
Signs to monitor
If you suspect your inflammation is linked to digestion, look for:
-
Immediate or post-prandial abdominal bloating
-
Visible food fragments in the stool
-
Brain fog after meals
4 – A special case: the role of gluten
“The role of gluten: Gluten exerts multiple harmful effects that compromise human health, not only in gluten-dependent diseases but also in chronic inflammatory conditions unrelated to gluten. After consumption, indigestible gluten peptides are modified by luminal microbial transglutaminase or transported across the intestinal epithelium to interact with the densely populated immune cells of the mucosa. As disruptors of intestinal permeability, undigested gluten peptides compromise the integrity of tight junctions, allowing foreign immunogenic molecules to reach internal compartments. Gliadin peptides are systemically distributed to remote organs, where they encounter endogenous tissue transglutaminase. Following post-translational deamidation or transamidation, the peptides become immunogenic and pro-inflammatory, inducing organ dysfunction and pathology. Cross-reactivity and sequence homology between gluten/gliadin peptides and human epitopes may contribute to molecular mimicry in the induction of autoimmunity. As proof of concept, gluten withdrawal alleviates disease activity in chronic inflammatory, metabolic, and autoimmune conditions, and even in neurodegeneration. We recommend combining a gluten-free diet with the Mediterranean diet to leverage the advantages of both. Before recommending gluten withdrawal for non–gluten-dependent conditions, patients should be asked about intestinal symptoms and screened for celiac-associated antibodies. The current list of gluten-induced diseases includes celiac disease, dermatitis herpetiformis, gluten ataxia, wheat allergy, and non-celiac gluten sensitivity. Given that gluten is a universal pro-inflammatory molecule, other non-celiac autoinflammatory and neurodegenerative conditions should be investigated for potential gluten elimination.” Gluten is a Proinflammatory Inducer of Autoimmunity. Aaron Lerner et al. Journal of Translational Gastroenterology 2024; 2(2):109–124. DOI: 10.14218/JTG.2023.00060.
Bibliographic references
-
Furman D, et al. Chronic inflammation in the etiology of disease across the life span. Nature Medicine. 2019.
A landmark review describing systemic chronic inflammation as a central trait in the major causes of global morbidity (cancer, cardiovascular disease, diabetes, chronic kidney disease, and others) and discussing social, environmental, and biological drivers. -
Franceschi C, et al. Inflamm-aging and immune-metabolic changes with aging. Cell. 2018.
This article introduces the concept of inflammaging—age-associated low-grade chronic inflammation—and highlights the role of persistent inflammatory mediators. -
Khanna D, Khanna S, et al. Obesity: A chronic low-grade inflammation and its markers. Journal of Inflammation Research. 2020.
A review analyzing obesity as a paradigmatic model of low-grade systemic inflammation, with extensive discussion of key inflammatory markers produced by adipose tissue. -
Chen L, et al. Inflammatory responses and inflammation-associated diseases in organs. Journal of Biomedical Research. 2017.
A comprehensive review of the molecular mechanisms of acute and chronic inflammatory responses and their implications in multiple systemic diseases (cardiovascular, metabolic, autoimmune, and neoplastic).
Back
