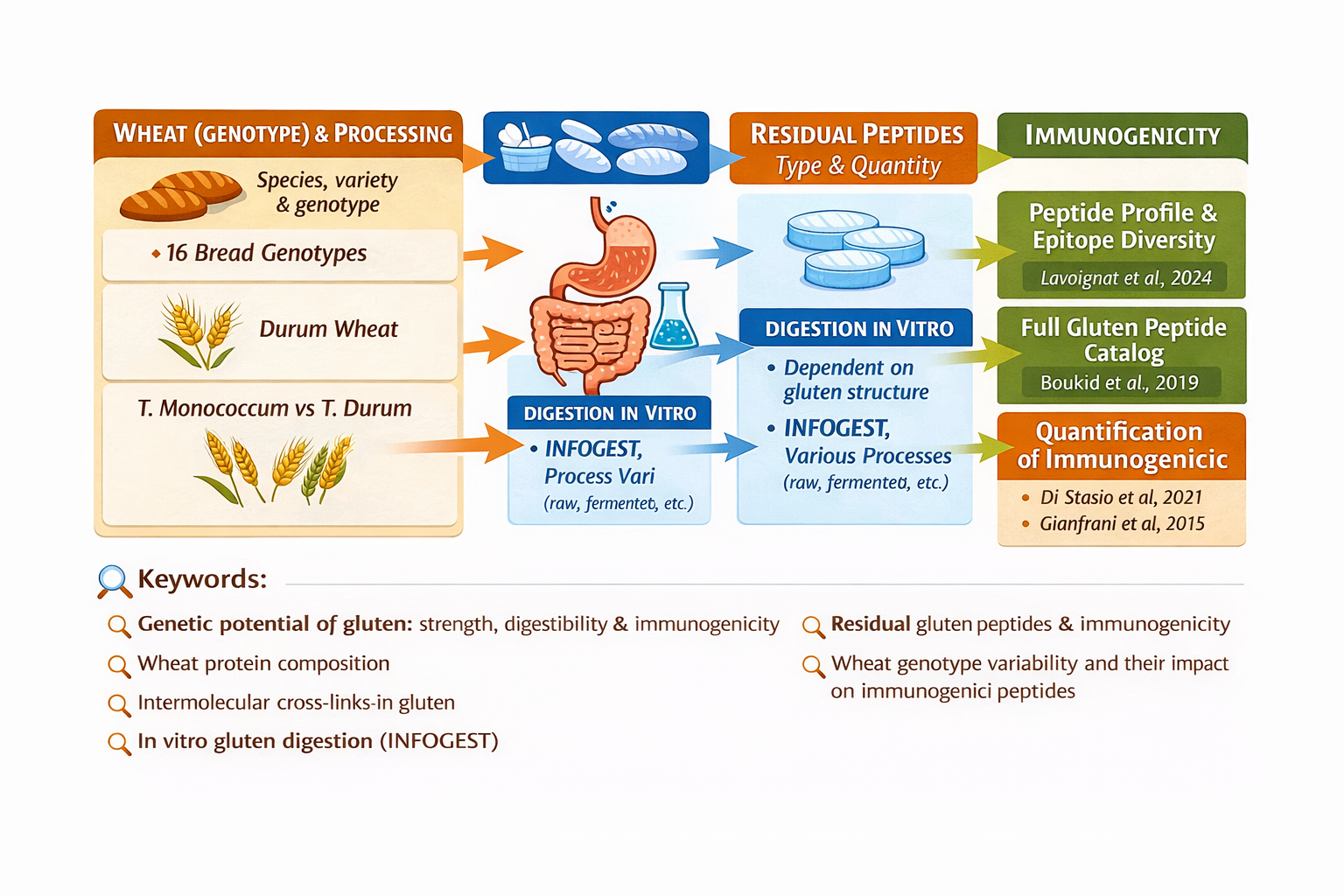
(Insight 2 of “Genetic Potential and Processing Conditions in the Determination of Gluten Strength, Digestibility, and Immunogenicity”)
The 33-mer peptide (sequence LQLQPFPQPQLPYPQPQLPYPQPQLPYPQPQPF) is recognized as one of the most digestion-resistant peptides derived from gluten proteins and as one of the main stimulators of T cells in the context of celiac disease.
Its importance stems from three key characteristics:
1 – Enzymatic resistance
Its high content of proline and glutamine makes it highly resistant to human digestive enzymes (pepsin, trypsin, chymotrypsin), allowing it to persist in the intestinal lumen after both in vitro and in vivo digestion.
2 – High immunogenicity
It contains multiple regions (epitopes) recognized by T cells from patients with celiac disease and was among the first peptides identified with this property.
3 – resence in common wheat species
It is present in most common hexaploid wheats (T. aestivum) and in spelt, but has been reported as absent in tetraploid/diploid wheats lacking the D genome (such as durum wheat, emmer, and einkorn).
For these reasons, the 33-mer peptide is frequently used as a marker for assessing “gluten immunogenicity” in flours and food products and for comparing wheat cultivars in research focused on immune response.
Key Findings from Studies on the 33-mer Peptide. Shan et al. (2002) — Identification and Immunogenicity of the 33-mer. Title: A resistant peptide from gliadin that is a potent activator of intestinal T cells in celiac disease. Authors: Shan L., Molberg Ø., Parrot I., Hausch F., Filiz F., Gray G.M., Sollid L.M., Khosla C. Journal: Science (2002). DOI: 10.1126/science.1074624
Core finding:
This landmark study isolated and characterized the 33-mer peptide as one of the most potent activators of T cells in celiac patients and demonstrated its extreme resistance to standard proteolytic digestion, confirming its immunogenic relevance.
Vader et al. (2002) — Structure and Epitopes of the 33-mer. Title: Structural basis for gluten intolerance in celiac sprue. Authors: Vader W., Stepniak D., Bunnik E., et al. Journal: Journal of Experimental Medicine (2002)
DOI: 10.1084/jem.20020609
Core finding:
Mapping of the major immunogenic epitopes within gliadins, explaining why sequences such as the 33-mer—with multiple and overlapping epitopes—are particularly active in triggering immune responses.
Schalk et al. (2017) — Quantification and Distribution of the 33-mer in Wheat. Title: Quantitation of the immunodominant 33-mer peptide from α-gliadin in wheat flours by liquid chromatography tandem mass spectrometry. Authors: Kathrin Schalk, Christina Lang, Herbert Wieser, Peter Koehler, Katharina Anne Scherf. Journal: Scientific Reports (2017). DOI: 10.1038/srep45092
Core finding:
This study measured the 33-mer content in a wide range of modern and ancient wheat flours using a targeted method (SIDA + LC-MS/MS), providing important data on variability among wheat genotypes.
Specific Findings from Schalk et al. (2017)
General overview:
The 33-mer peptide was detected in all common wheat (hexaploid) and spelt flours analyzed.
Reported values ranged approximately from 90.9 μg/g to 602.6 μg/g of flour.
The peptide was not detected (below limit of detection) in cereals lacking the D genome such as durum wheat, emmer, and einkorn, consistent with the absence of α2-gliadins encoding this peptide.
Interpretation:
The observed variability indicates that even within closely related wheat types, the amount of 33-mer peptide can differ substantially. This suggests that genotype and cultivar variation have a tangible impact on the content of celiac-related immunogenic peptides.
Related and Complementary Evidence
Norwig et al. (2024) confirm the presence of the 33-mer in all analyzed common wheat and spelt samples, reinforcing its central role in gluten-related peptidomic research.
Broader proteomic and peptidomic approaches show that the 33-mer is only one of several immunogenic peptides that can persist after digestion, but it remains a robust marker for comparing genotypes and technological processes (fermentation, baking, etc.).
Explanatory Box — Main Results from Schalk et al. (2017)
33-mer peptide content (μg/g flour) in analyzed wheats:
Minimum observed value: ~90.9 μg/g
Maximum observed value: ~602.6 μg/g
Typical distribution: most samples fall in the 200–400 μg/g range
Absence: not detected in durum wheat, emmer, and einkorn, likely due to the lack of D-genome α2-gliadin.
Why This Subsection Completes the Big Picture
Starting from a clear biological concept (resistance + immunogenicity), this subsection connects:
Molecular mechanisms (multiple epitopes within a single peptide),
Classical experimental evidence,
Real quantitative data across different cultivars,
Consistency with variability observed in broader peptidomic studies.
This provides readers with a solid framework to understand not only that the 33-mer exists, but why its presence and quantity vary among wheats and why it matters for digestion and immune response.
Keywords: 33-mer peptide, gluten immunogenicity, celiac disease gluten peptides, α-gliadin peptides, digestion-resistant gluten peptides, wheat cultivars immunogenicity, gluten T-cell epitopes, gluten peptidomics, wheat genetics and celiac disease, gluten digestibility