Le omega gliadine, soprattutto la omega-5 gliadina termostabile, sono responsabili dell’anafilassi grano-dipendente indotta dall’esercizio fisico (wheat-dependent exercise-induced anaphylaxis, WDEIA) diffusa principalmente tra gli adulti.
“Wheat [Triticum aestivum (T.a.)] ingestion can cause a specific allergic reaction, which is called wheat-dependent exercise-induced anaphylaxis (WDEIA). The major allergen involved is ω-5 gliadin, a gluten protein coded by genes located on the B genome. Our aim was to study the immunoreactivity of proteins in Triticum monococcum (einkorn, T.m.), a diploid ancestral wheat lacking B chromosomes, for possible use in the production of hypoallergenic foods. A total of 14 patients with a clear history of WDEIA and specific immunoglobulin E (IgE) to ω-5 gliadin were enrolled. Skin prick test (SPT) with a commercial wheat extract and an in-house T.a. gluten diagnostic solution tested positive for 43 and 100% of the cases, respectively. No reactivity in patients tested with solutions prepared from four T.m. accessions was observed. The immunoblotting of T.m. gluten proteins performed with the sera of patients showed different IgE-binding profiles with respect to T.a., confirming the absence of ω-5 gliadin. A general lower immunoreactivity of T.m. gluten proteins with scarce cross-reactivity to ω-5 gliadin epitopes was assessed by an enzyme-linked immunosorbent assay (ELISA). Given the absence of reactivity by SPT and the limited cross-reactivity with ω-5 gliadin, T.m. might represent a potential candidate in the production of hypoallergenic bakery products for patients sensitized to ω-5 gliadin. Further analyses need to be carried out regarding its safety”. Study on the Immunoreactivity of Triticum monococcum (Einkorn) Wheat in Patients with Wheat-Dependent Exercise-Induced Anaphylaxis for the Production of Hypoallergenic Foods. Lombardo Cet altri J Agric Food Chem. 2015
Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction?
Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction?
Roberto De Giorgio, Umberto Volta, Peter R Gibson. Published Online First 15 June 2015. Gut 2016; 65:169–178.
Riassunto
La sindrome dell’intestino irritabile (IBS) è uno dei tipi più comuni di disturbo funzionale intestinale. Una crescente attenzione è stata data al ruolo causale del cibo nell’IBS. L’ingestione di cibo fa precipitare o aggrava i sintomi, come dolore addominale e gonfiore nei pazienti con IBS attraverso diversi meccanismi ipotizzati tra cui l’attivazione immunitaria e dei mastociti, la stimolazione dei meccanorecettori e l’attivazione chemosensoriale. Il grano è considerato uno dei fattori scatenanti dell’IBS più rilevanti, anche se i componenti di questo cereale coinvolti rimangono sconosciuti. Il glutine, altre proteine, del grano, ad esempio gli inibitori dell’amilasi-tripsina e i fruttani (questi ultimi appartenenti a oligo-di-mono-saccaridi e polioli fermentabili = FODMAP), sono stati identificati come possibili fattori per la generazione / esacerbazione dei sintomi. Questa incertezza sul vero colpevole o colpevoli ha aperto uno scenario di definizioni semantiche favorite dai risultati discordanti degli studi controllati in doppio cieco controllati con placebo, che hanno generato vari termini che vanno dalla sensibilità al glutine non celiaca a quella più ampia del grano non celiaco o sensibilità alle proteine del grano o, persino, sensibilità FODMAP. Il ruolo dei FODMAP nel suscitare il quadro clinico dell’IBS va oltre, poiché questi carboidrati a catena corta si trovano in molti altri componenti dietetici, tra cui frutta e verdura. In questa recensione, abbiamo valutato la letteratura attuale al fine di scoprire se la sensibilità al glutine / grano / FODMAP rappresenti “fatti” e non “fiction” nei sintomi dell’IBS. Questa conoscenza dovrebbe promuovere la standardizzazione nelle strategie dietetiche (senza glutine / senza grano e FODMAP basso) come misure efficaci per la gestione dei sintomi IBS.
ABSTRACT
IBS is one of the most common types of functional bowel disorder. Increasing attention has been paid to the causative role of food in IBS. Food ingestion precipitates or exacerbates symptoms, such as abdominal pain and bloating in patients with IBS through different hypothesised mechanisms including immune and mast cell activation, mechanoreceptor stimulation and chemosensory activation. Wheat is regarded as one of the most relevant IBS triggers, although which component(s) of this cereal is/are involved remain(s) unknown. Gluten, other wheat proteins, for example, amylase-trypsin inhibitors, and fructans (the latter belonging to fermentable oligo-di-mono-saccharides and polyols (FODMAPs)), have been identified as possible factors for symptom generation/exacerbation. This uncertainty on the true culprit(s) opened a scenario of semantic definitions favoured by the discordant results of double-blind placebo-controlled trials, which have generated various terms ranging from non-coeliac gluten sensitivity to the broader one of non-coeliac wheat or wheat protein sensitivity or, even, FODMAP sensitivity. The role of FODMAPs in eliciting the clinical picture of IBS goes further since these short-chain carbohydrates are found in many other dietary components, including vegetables and fruits. In this review, we assessed current literature in order to unravel whether gluten/wheat/FODMAP sensitivity represent ‘facts’ and not ‘fiction’ in IBS symptoms. This knowledge is expected to promote standardisation in dietary strategies (gluten/wheat-free and low FODMAP) as effective measures for the management of IBS symptoms.
Extract from study:
WHEAT SENSITIVITY
Wheat is considered one of the foods known to evoke IBS symptoms. However, which component(s) of wheat is/are actually responsible for these clinical effects still remain(s) an unsettled issue. The two parts of wheat that are thought to have a mechanistic effect comprise proteins (primarily, but not exclusively, gluten) and carbohydrates (primarily indigestible short-chain components, FODMAPs). Two distinct views characterise the clinical debate: one line identifies wheat proteins as a precipitating/perpetuating factor leading to symptoms, while the other believes that FODMAPs are the major trigger for IBS.
The controversy over nomenclature
If gluten is a major trigger for IBS, it expands the gluten-related disorders by adding a new entity now referred to as non-coeliac gluten sensitivity (NCGS). Indeed, coeliac disease-like abnormalities were reported in a subgroup of patients with IBS many years ago. A recent expert group of researchers reached unanimous consensus attesting the existence of a syndrome triggered by gluten ingestion. This syndrome recognises a wide spectrum of symptoms and manifestations including an IBS-like phenotype, along with an extra-intestinal phenotype, that is, malaise, fatigue, headache, numbness, mental confusion (‘brain fog’), anxiety, sleep abnormalities, fibromyalgia-like symptoms and skin rash. In addition, other possible clinical features include gastroesophageal reflux disease, aphthous stomatitis, anaemia, depression, asthma and rhinitis. Symptoms or other manifestations occur shortly after gluten consumption and disappear or recur in a few hours (or days) after gluten withdrawal or challenge. A fundamental prerequisite for suspecting NCGS is to rule out all the established gluten/wheat disorders, comprising coeliac disease (CD), gluten ataxia, dermatitis herpetiformis and wheat allergy. The major issue not addressed by the consensus opinion was that gluten is only one protein contained within wheat. Other proteins, such as amylase-trypsin inhibitors (ATIs), are strong activators of innate immune responses in monocytes, macrophages and dendritic cells. Furthermore, wheat germ agglutinin, which has epithelial-damaging and immune effects at very low doses at least in vitro, might also contribute to both intestinal and extraintestinal manifestations of NCGS. Consequently, a further development of this research field led to suggestions of a broader term, non-coeliac wheat sensitivity (NCWS). The problems with this term are twofold. First, rye and barley may be inappropriately excluded. Second, the term will refer to any wheat component that might be causally related to induction of symptoms and, therefore, will also include fructans (FODMAPs). It will then have a very nonspecific connotation in IBS. A more correct term would then be non-coeliac wheat protein sensitivity (NCWPS) since this does not attribute effects to gluten without evidence of such specificity, eliminates the issue of fructan-induced symptoms and avoids the unknown contribution of rye and barley proteins to the symptoms. Both NCGS, the currently accepted term, and NCWPS will be used subsequently in this paper.
Grano monococco: perchè è così importante
Riassunto delle principali caratteristiche del grano monococco che gli conferiscono grande potenzialità per essere utilizzato per la preparazione di prodotti da forno salati ma anche dolci per le persone che:
• sono geneticamente predisposte per la celiachia (1) (2) (3) (4) (5),
• debbono tenere sotto controllo l’indice glicemico (6),
• sensibili al glutine non celiache, reintroducono il glutine dopo la sua esclusione (7),
• hanno difficoltà con la digestione del glutine (8).
• sono sensibili alle ATI -amylase trypsina inibitors-. (9)
Da sottolineare, anche, le elevate qualità nutrizionali del grano monococco (10).
(1)- Immunogenicity of monococcum wheat in celiac patients
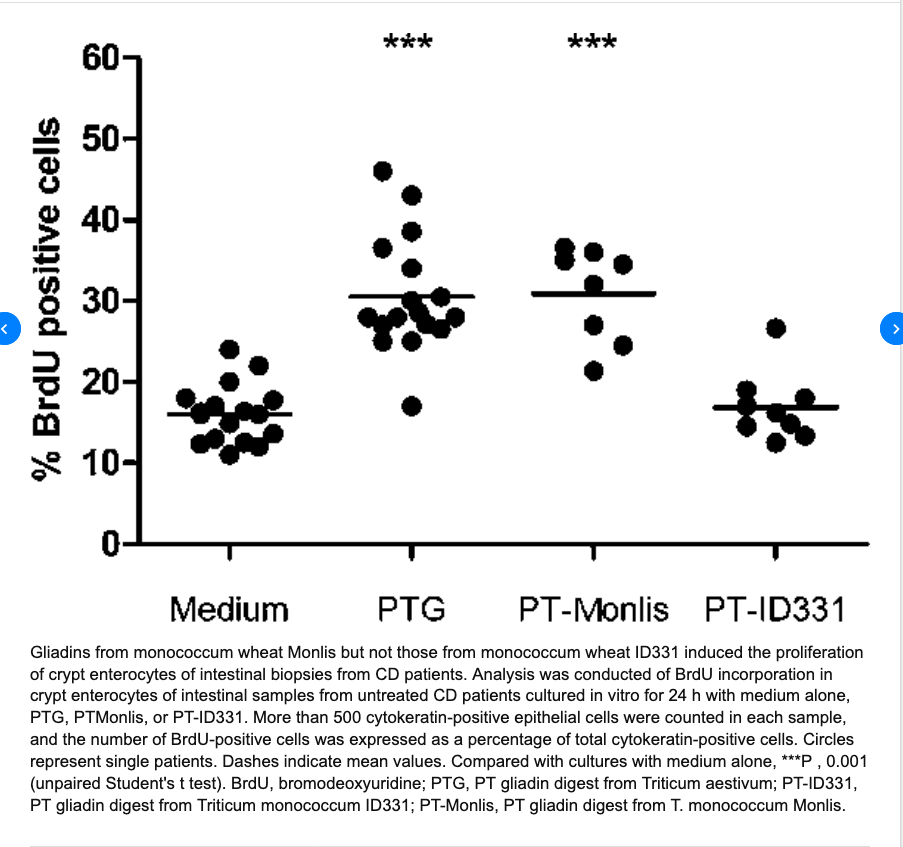
………..omissis. “Conclusions: Our data show that the monococcum lines Monlis and ID331 activate the CD T cell response and suggest that these lines are toxic for celiac patients. However, ID331 is likely to be less effective in inducing CD because of its inability to activate the innate immune pathways”. Immunogenicity of monococcum wheat in celiac patients. Carmen Gianfrani et altri. Am J Clin Nutr 2012;96:1339–45.
(2) ………omissis. “D’altra parte, tenuto conto che l’incidenza e la gravità della celiachia dipende dalla quantità e dalla nocività delle prolamine e che alcuni genotipi di grano monococco hanno una elevata qualità panificatoria accoppiata con assenza di citotossicità e ridotta immunogenicità, è atteso che l’uso delle farine di monococco nella dieta della popolazione generale, all’interno della quale si trova una elevata percentuale di individui predisposti geneticamente alla celiachia ma non ancora celiaci, possa contribuire a contenere la diffusione di questa forma di intolleranza alimentare. Ciò lascia pensare che il grano monococco, riportato recentemente in coltivazione in Italia dai ricercatori del Consiglio per la Ricerca e la sperimentazione in Agricoltura (CRA) di Roma e San Angelo Lodigiano, potrà svolgere un ruolo importante nella prevenzione della celiachia, sia direttamente sotto forma di pane e pasta sia indirettamente come specie modello per lo studio del ruolo dell’immunità innata nell’insorgenza della celiachia”. Le nuove frontiere delle tecnologie alimentari e la celiachia Norberto Pogna, Laura Gazza (2013).
(3)-Extensive in vitro gastrointestinal digestion markedly reduces the immune-toxicity of Triticum monococcum wheat: Implication for celiac disease
Carmen Gianfrani, Alessandra Camarca, Giuseppe Mazzarella, Luigia Di Stasio, Nicola Giardullo, Pasquale Ferranti, Gianluca Picariello, Vera Rotondi Aufiero, Stefania Picascia, Riccardo Troncone, Norberto Pogna, Salvatore Auricchio
and Gianfranco Mamone. Mol. Nutr. Food Res. 2015, 00, 1–11
Scope: The ancient diploid Triticum monococcum is of special interest as a candidate low-toxic wheat species for celiac disease patients. Here, we investigated how an in vitro gastro-intestinal digestion, affected the immune toxic properties of gliadin from diploid compared to hexaploid wheat.
Method and results: Gliadins from Triticum monococcum, and Triticum aestivum cultivars were digested using either a partial proteolysis with pepsin-chymotrypsin, or an extensive degradation that used gastrointestinal enzymes including the brush border membrane enzymes. The immune stimulatory properties of the digested samples were investigated on T-cell lines and jejunal biopsies from celiac disease patients. The T-cell response profile to the Triticum mono coccum gliadin was comparable to that obtained with Triticum aestivum gliadin after the partial pepsin-chymotrypsin digestion. In contrast, the extensive gastrointestinal hydrolysis drastically reduced the immune stimulatory properties of Triticum monococcum gliadin. MS-based analy- sis showed that several Triticum monococcum peptides, including known T-cell epitopes, were degraded during the gastrointestinal treatment, whereas many of Triticum aestivum gliadin survived the gastrointestinal digestion.
Conclusion: he pattern of Triticum monococcum gliadin proteins is sufficiently different from those of common hexaploid wheat to determine a lower toxicity in celiac disease patients following in vitro simulation of human digestion.
(4) …….omissis. “Abstract. A growing interest in developing new strategies for preventing coeliac disease has motivated efforts to identify cereals with null or reduced toxicity. In the current study, we investigate the biological effects of ID331 Triticum monococcum gliadin-derived peptides in human Caco-2 intestinal epithelial cells. Triticum aestivum gliadin derived peptides were employed as a positive control. The effects on epithelial permeability, zonulin release, viability, and cytoskeleton reorganization were investigated. Our findings confirmed that ID331 gliadin did not enhance permeability and did not induce zonulin release, cytotoxicity or cytoskeleton reorganization of Caco-2 cell monolayers. We also demonstrated that ID331 ω-gliadin and its derived peptide ω(105–123) exerted a protective action, mitigating the injury of Triticum aestivum gliadin on cell viability and cytoskeleton reorganization. These results may represent a new opportunity for the future development of innovative strategies to reduce gluten toxicity in the diet of patients with gluten intolerance”. Protective effects of ID331 Triticum monococcum gliadin on in vitro models of the intestinal epithelium. Giuseppe Jacomino et altri 2016.
