Il cibo non digerito e il microbiota intestinale possono collaborare nella patogenesi delle malattie neuroinfiammatorie: una questione di barriere e una proposta sull’origine della specificità d’organo
Premessa
La digeribilità dei prodotti realizzati con farina di grano è andata mano mano diminuendo in relazione alla sempre più diffusa necessità di grani che diano un impasto adatto ai processi industriali. La digeribilità del cibo e, dunque in particolare dei grani è rilevante in quanto in molte persone concorre in modo spesso significativo ad aumentare l’infiammazione intestinale. Lo studio proposto affronta questa importante tematica.
Undigested Food and Gut Microbiota May Cooperate in the Pathogenesis of Neuroinflammatory Diseases: A Matter of Barriers and a Proposal on the Origin of Organ Specificity . Paolo Riccio, Rocco Rossano Nutrients. 2019 Nov 9;11(11):2714. doi: 10.3390/nu11112714.
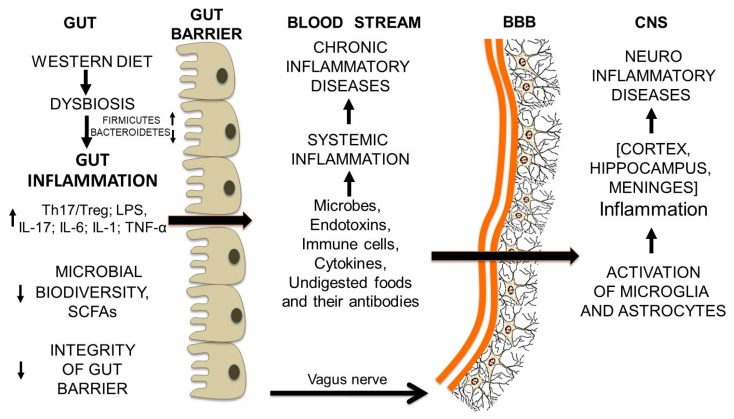
Abstract: As food is an active subject and may have anti-inflammatory or pro-inflammatory effects, dietary habits may modulate the low-grade neuroinflammation associated with chronic neurodegenerative diseases. Food is living matter different from us, but made of our own nature. Therefore, it is at the same time foreign to us (non-self), if not yet digested, and like us (self), after its complete digestion. To avoid the efflux of undigested food from the lumen, the intestinal barrier must remain intact. What and how much we eat shape the composition of gut microbiota. Gut dysbiosis, as a consequence of Western diets, leads to intestinal inflammation and a leaky intestinal barrier. The efflux of undigested food, microbes, endotoxins, as well as immune-competent cells and molecules, causes chronic systemic inflammation. Opening of the blood-brain barrier may trigger microglia and astrocytes and set up neuroinflammation. We suggest that what determines the organ specificity of the autoimmune-inflammatory process may depend on food antigens resembling proteins of the organ being attacked. This applies to the brain and neuroinflammatory diseases, as to other organs and other diseases, including cancer. Understanding the cooperation between microbiota and undigested food in inflammatory diseases may clarify organ specificity, allow the setting up of adequate experimental models of disease and develop targeted dietary interventios.
Keywords: Alzheimer’s disease; Parkinson’s disease; amyotrophic lateral sclerosis; autism spectrum disorders; blood-brain barrier; diet; gut microbiota; inflammation; intestinal barrier; multiple sclerosis (traduzione abstract in fondo articolo)
In evidenza questo passaggio:
omissis. 7. What Food Is and Why It must be Digested Food is what we eat: everything that has to do with the matter of life, not inorganic matter. We do do not eat sand, mud, paper or plastic, but everything we recognize to be safe and in its essence similar to us, i.e., that which is made like us and that we know how to “treat”, metabolize and and transform in order to obtain energy or to replace our altered constituents over time. Therefore, our food is made up food is made up exclusively of living matter (which has often been inactivated). However, when we consume it, food is completely different from us (non-self) and we cannot use use any of it as it is. Altogether, dietary macromolecules are so different from us that we must provide for for their elimination as soon as they occur outside the gastrointestinal system. Although the biological cells and the macromolecular structures present in our menus (proteins, membranes, polysaccharides) are different from ours, their basic constituents [the bioelements (C,N,O,H), and simple molecules such as fatty acids, monosaccharides, aminoacids] are the same as those we use (Figure 5). Ultimately, living matter is at the same time both foreign to us (non-self) and those we use (Figure 5) and congenial to us (self). As they are different in origin from ours, tissues, cells and proteins from food cannot be used as they are. They must be degraded to simple molecules by the digestive system in the gastro-intestinal tract (the reaction vessel) and then absorbed. This is why food must be digested before being absorbed: it is non-self before digestion and becomes self when digestion is complete. Only the completely digested molecules are congenial to us, are recognized as self and can enter our metabolism after their absorption. In conclusion the task of In digestion is to make food like us, while absorption is required to make absorption simple molecules available to our metabolism. In just over a day (35–40h) our food becomes part of us (Figuren 6).
Figure 1. Chronic neurodegenerative diseases have a chronic inflammatory basis in common.
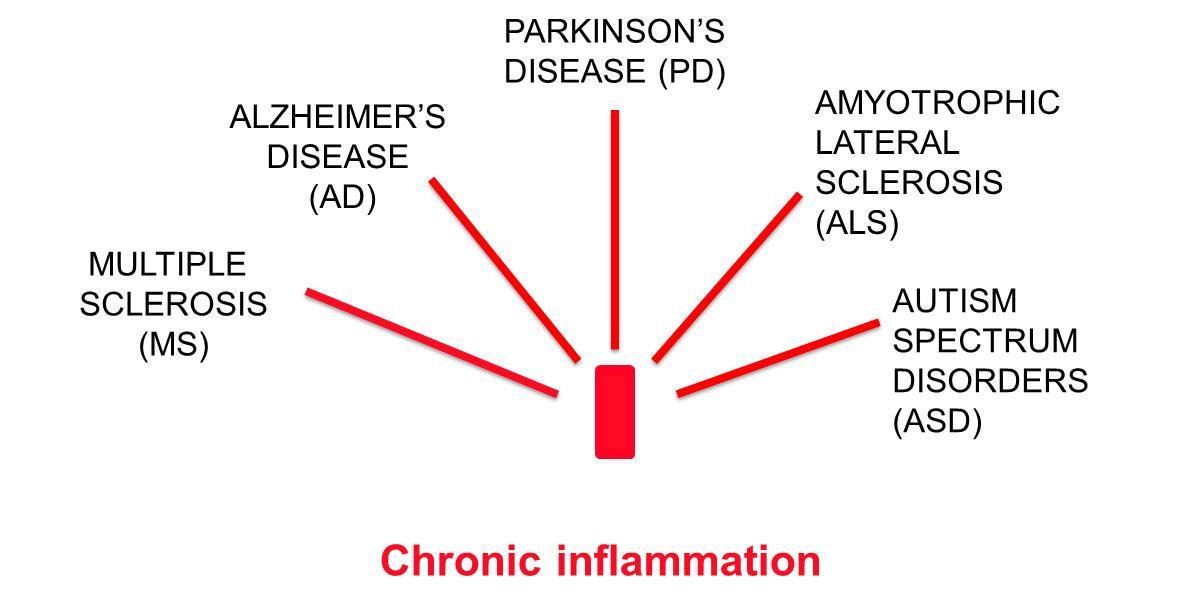
Figure 2 Dietary habits affect both our metabolism and the composition of our gut microbiota.
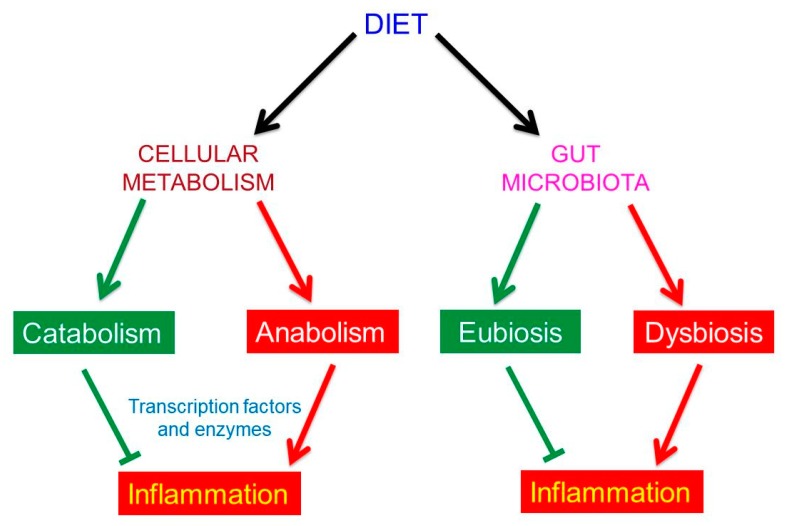
Figure 3 Pro-inflammatory dietary factors.
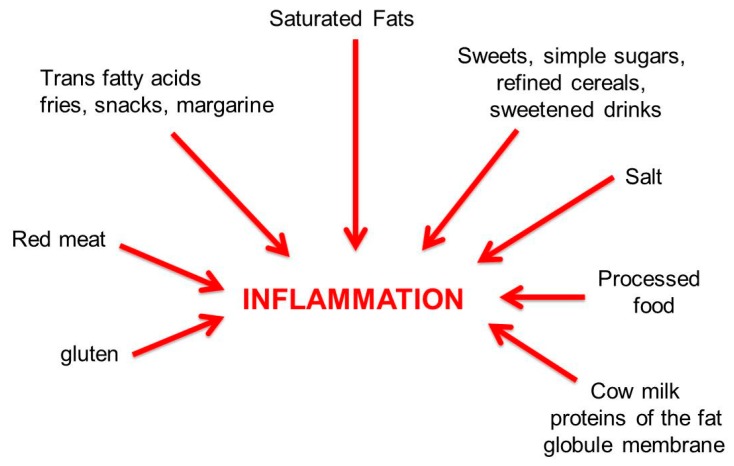
Figure 4 Anti-inflammatory dietary factors. The intrinsic factors are those playing a role in our metabolism. They include: omega-3 poly-unsaturated long-chain fatty acids (n-3 PUFAs), present in fish oil; vitamins A and D, B12, PP, E and C; oligoelements such as magnesium, zinc and selenium; thiolic acids such as alfa-lipoic acid (ALA), N-acetyl cysteine and glutathione. The extrinsic factors are the polyphenols, the phytochemicals present in vegetables: they have anti-inflammatory properties and upregulate the catabolism, but are recognized by our metabolism as “foreign” molecules. However, as shown below, they represent a food source for the gut microbiota. Prebiotics and probiotics are cited here for their anti-inflammatory action, but their effects are exerted mainly through the gut microbiota.
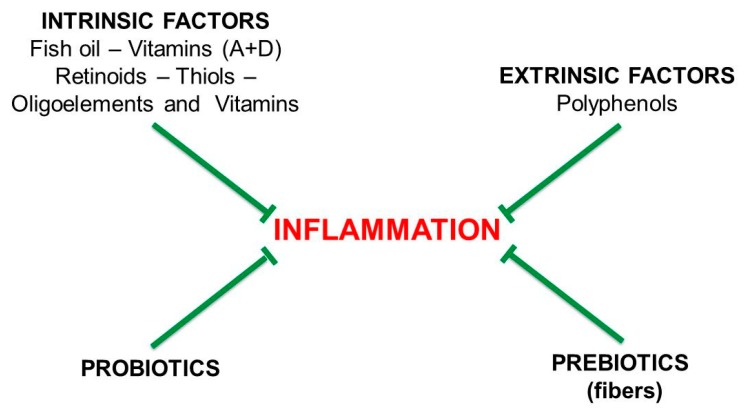
Figure 5 The basic constituents of living matter. The world we know is made up of 92 chemical elements, 81 of which are stable. Living matter uses only about 26–30 of these elements, but 99% of it consists of only four “bioelements”: carbon (C); nitrogen (N); oxygen (O); and hydrogen (H). The bioelements are able to form 4-3-2-1 bonds, respectively, and have a high tendency to get together and form complex molecules such as proteins and nucleic acids, which are different for every species. This means that at the basic level all living organisms are equal to each other, while in their complex forms they are different.
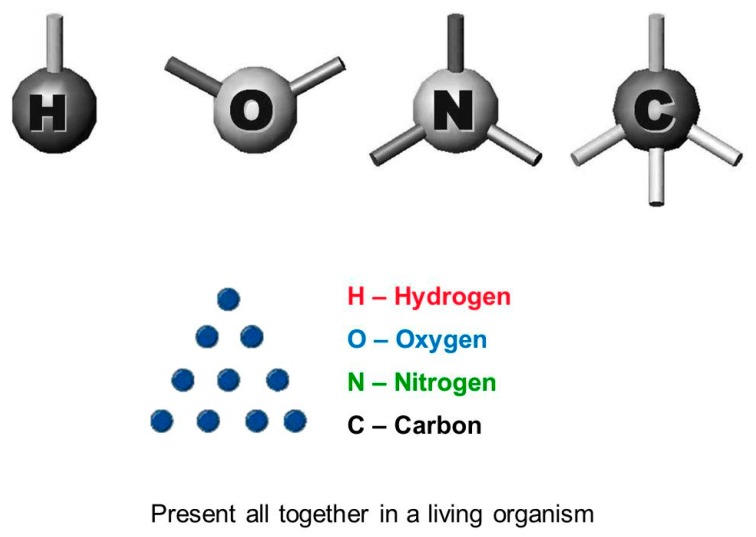
Figure 6 Schematic representation of the metabolic processes, from digestion of the simplest molecules, common to all living organisms and to their fruition.
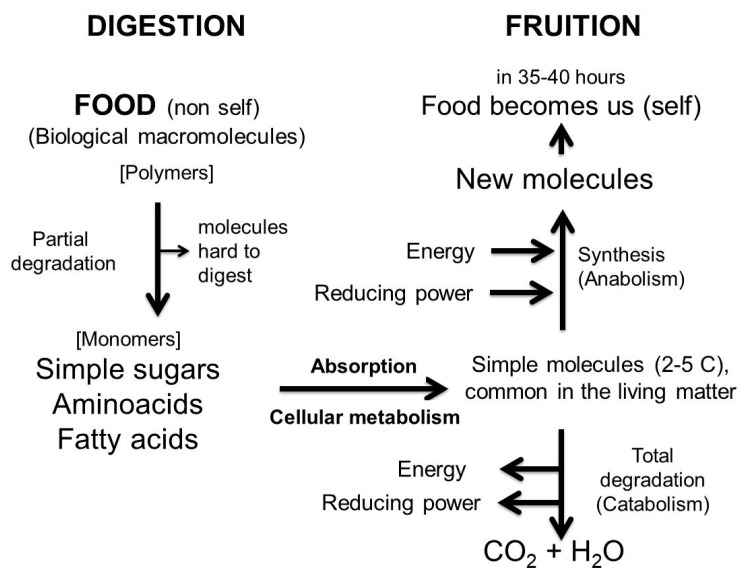
Figure 7 Effects of dietary factors and stressors on the integrity of the intestinal barrier.
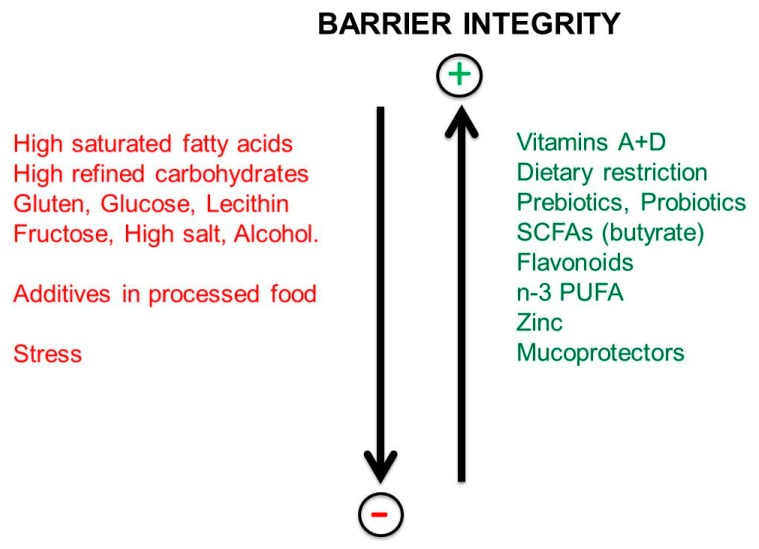
Figure 8 From Westernized dietary habits to neuroinflammation and neurodegenerative diseases: a schematic representation.
Abstract: traduzione
Poiché il cibo è un soggetto attivo e può avere effetti antinfiammatori o pro-infiammatori, le abitudini alimentari possono modulare la neuroinfiammazione di basso grado associata a malattie neurodegenerative croniche. Il cibo è materia vivente diversa da noi, ma fatta della nostra stessa natura. Pertanto, è al tempo stesso estraneo a noi (non self=estraneo) se non ancora digerito e come noi (self=se stesso) dopo la sua completa digestione. Per evitare l’efflusso di cibo non digerito dal lume (stomaco/intestino), la barriera intestinale deve rimanere intatta. Cosa e quanto mangiamo modella la composizione del microbiota intestinale. La disbiosi intestinale, come conseguenza delle diete occidentali, porta a un’infiammazione intestinale e una barriera intestinale cheperde la sua integrità. L’efflusso di cibo non digerito, microbi, endotossine, nonché cellule e molecole immunocompetenti provoca un’infiammazione sistemica cronica. L’apertura della barriera ematoencefalica può innescare microglia e astrociti e impostare neuroinfiammazione. Suggeriamo che ciò che determina la specificità d’organo del processo autoimmune-infiammatorio può dipendere da antigeni alimentari simili alle proteine dell’organo che viene attaccato. Questo vale per il cervello e le malattie neuroinfiammatorie, come per altri organi e altre malattie, compreso il cancro. Comprendere la cooperazione tra microbiota e cibo non digerito nelle malattie infiammatorie può chiarire la specificità dell’organo, consentire la creazione di adeguati modelli sperimentali di malattia e sviluppare interventi dietetici mirati.
Autorizzazione: Deed Creative Commons Attribuzione 4.0 Internazionale (CC BY 4.0)
